Permacath insertion is a minimally invasive procedure in which a catheter is placed into a blood vessel in the neck or upper chest. This catheter is used for hemodialysis, a vital treatment for patients with kidney disease.
Fistuloplasty is a minimally invasive procedure used to clear blockages in an arteriovenous fistula, enabling access for dialysis without the need for surgery. The blockage is treated by inflating a specialized balloon or device, which improves blood flow through the fistula.
TEVAR is a minimally invasive procedure used to treat conditions affecting the thoracic aorta, such as aneurysms or dissections. Located in the chest, the thoracic aorta is a critical blood vessel, and TEVAR offers a less invasive alternative to open surgery, providing benefits like shorter hospital stays and faster recovery times.
A peripheral angiogram, also known as extremity angiography, is a diagnostic test that uses X-rays and contrast dye to identify narrowed or blocked arteries supplying blood to the legs, feet, arms, or hands.
Deep vein thrombosis (DVT) is a condition where a blood clot forms in a vein located deep within the body, most commonly in the legs, arms, or other areas.
Varicocele embolization is a minimally invasive, non-surgical procedure designed to treat varicoceles—enlarged veins in the scrotum. It is an effective option for addressing varicoceles that cause pain, swelling, or infertility.
Varicose veins are enlarged, twisted veins that typically appear on the legs due to increased pressure on the veins. This condition is caused by the weakening of vein walls or malfunctioning valves, which leads to improper blood flow.
VenaSeal provides fast and effective relief from varicose veins. This minimally-invasive, outpatient procedure offers a more comfortable experience with shorter recovery times.
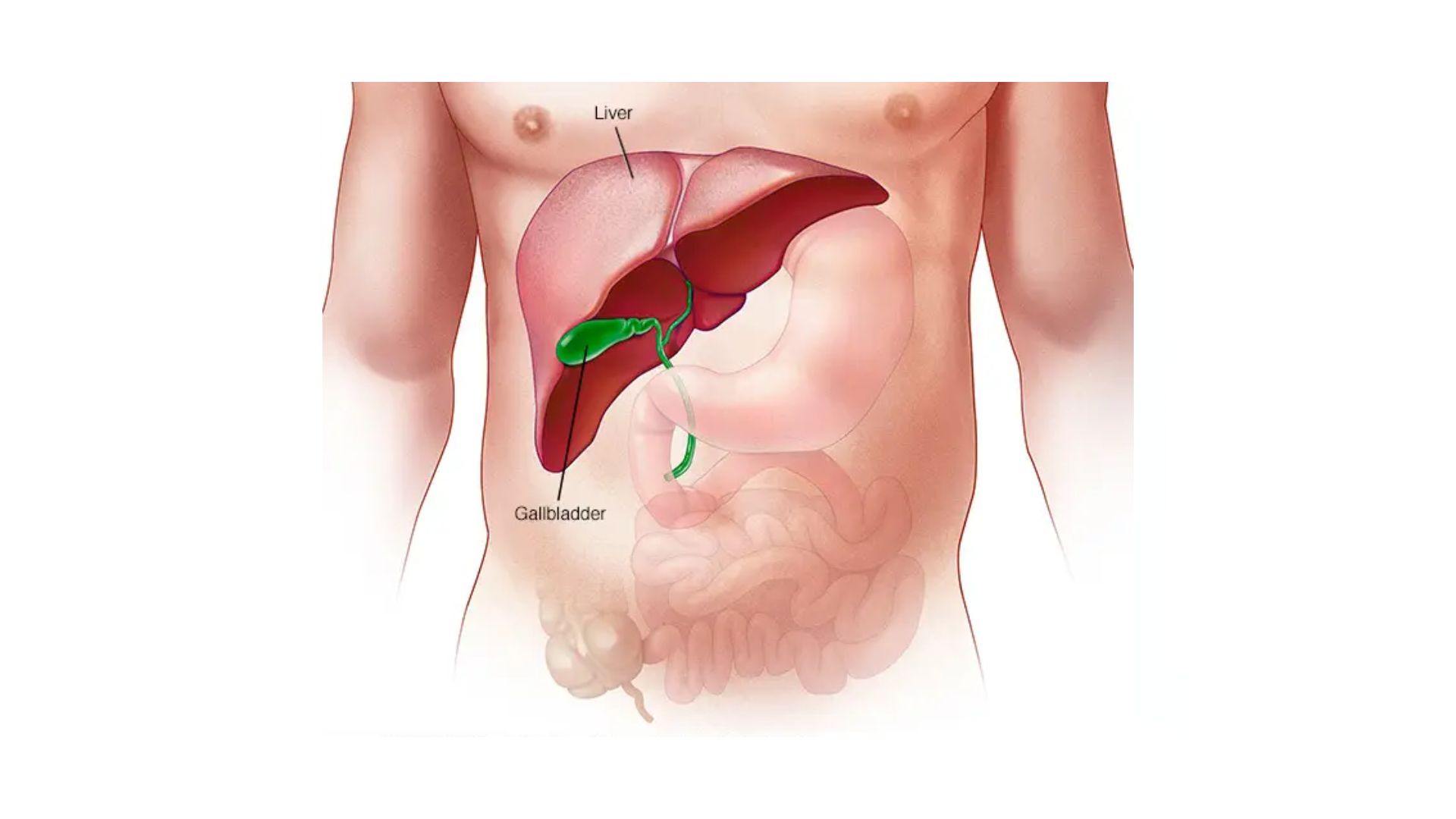
Liver Cirrhosis and PHT
What is it?

- A transjugular intrahepatic portosystemic shunt (TIPS) is a percutaneously created connection within the liver between the portal and systemic circulations.
- It is placed to reduce portal pressure in patients with complications related to portal hypertension.
- This procedure has emerged as a less invasive alternative to surgery in patients with end-stage liver disease.
- The goal of TIPS placement is to divert portal blood flow into the hepatic vein, so as to reduce the pressure gradient between portal and systemic circulations.
- Shunt patency is maintained by placing an expandable metal stent across the intrahepatic tract
- Patient has to take lifelong blood thinner in some condition like buddchiari syndrome.


Why (Indications)?
- Acute variceal bleeding that cannot be successfully controlled with medical treatment, including sclerotherapy.
- Recurrent and refractory variceal bleeding
- Therapy for refractory ascites.
- Portal decompression in patients with hepatic venous outflow obstruction (Budd-Chiari syndrome) or hepatorenal syndrome.
Why Not (Contraindication)?
- Absolute contraindications:
- Right-sided heart failure with increased central venous pressure
- Polycystic liver disease
Relative contraindications:
- Active intrahepatic or systemic infection
- Severe hepatic encephalopathy poorly controlled with medical therapy
- Hyper vascular hepatic tumors
- PV thrombosis
What you are to do before procedure (Preparation)?
- Visit us in OPD (9-5) with previous lab results (*CBC, LFT, Serum Creatinine, PT/INR), imaging etc.
- If you are on blood thinner like Aspirin inform during appointment.
- Get admission one day prior to scheduled procedure.
- One accompanying person
- Need to sign a consent form for procedure
- Cash or ATM card
Approx. Stay in hospital?
We have very fast and competent working team (Consultant, fellow, clinical assistant, technician and ward assistant) which provide you comfortable atmosphere and ease your nerves. Usual time of stay is around 2-3 Days.
Complications:
- Obstruction to flow
- Shunt obstruction (38%)
- Hepatic vein stenosis
- Trauma
- Vascular injury
- Biliary injury
- Stent dislodgment
Resume to work?
You can resume your work after 1 week if existing disease allows.
Results: When and How?
Follow-up Doppler after 3 days, 7days, 1 month than every 3-6 month.
For any Queries or Appointment please call
What is it?
- Balloon-occluded retrograde transvenous obliteration (BRTO) has been introduced as a treatment method that aims to directly obliterate the GVA.
- The technical difficulty of BRTO relies on the anatomy of the afferent and draining veins of the GV.
- In most cases, there is a gastrorenal or gastrocaval shunt. In this situation under fluoroscopic guidance, a balloon catheter is inserted into the outlet of the gastrorenal or gastrocaval shunt through a sheath placed in the right femoral vein.
- Immediately afterward, venography is performed with an injection of 10–15 mL contrast medium via the inflated balloon catheter, and GV are slowly, intermittently, and completely filled with a sclerosant.


Why (Indications)?
When TIPS cannot be offered :
- Encephalopathy
- Poor hepatic reserve (MELD>18)
- Failed TIPS
- Coagulopathy
Absence of global complications of PHT like ascites, hydrothorax, PHG ? Primary prophylaxis for isolated gastric varices
Why Not (Contraindication)?
What you are to do before procedure (Prepration)?
- Visit us in OPD (9-5) with Referring Doctor prescription, previous lab results (*CBC,LFT, Serum Creatinine, PT/INR),imaging etc.
- If you are on blood thinner like Asprin inform during appointment.
- Get admission one day prior to scheduled procedure.
- One accompanying person
- Need to sign a consent form for procedure
Approx Stay in hospital ?
We have very fast and competent working team (Consultant, fellow,clinical assistant, technician and ward assistant) which provide you comfortable atmosphere and ease your nerves. Usual time of stay is around 1-2 Days.
Complications:
Epigastric and back pain, fever and transient hematuria are the most common complications of BRTO.
Resume to work?
You can resume your work after 2-3 days if existing disease allows.
Results: When and How?
Follow-up Endoscopy and CT scan after 3 days.
For any Queries or Appointment please call
